
Helpful tips for living
with sickle cell disease

Managing sickle cell disease may feel overwhelming, but the following tips may help:



Prepare for doctor visits by keeping notes on any concerns or questions you have ahead of time. Then speak up and be honest when talking to the doctor.
When it comes to managing your sickle cell disease, it is important to be open and honest with your doctor.
If you are the parent or caregiver of a child with sickle cell disease, having a transition plan can help navigate into adult care. Working with doctors and other health care providers may help with the transition process.
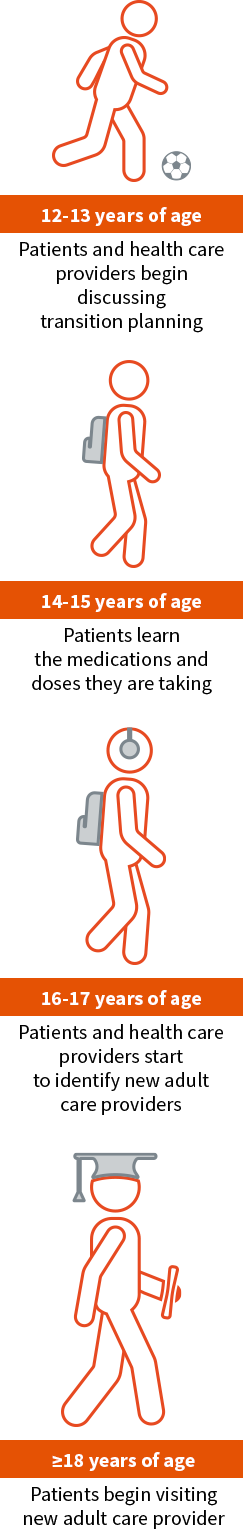
Tips for speaking with your child's paediatrician about transitioning:
People with sickle cell disease may feel less burdened when they have family and friends they can depend on. Don’t underestimate the help others can provide.
More sickle cell research has led to a better understanding of the underlying causes of the condition and the creation of possible therapies. Remember, you’re not alone. There are support groups for people affected by sickle cell disease all around the world. Need help finding one? Ask your doctor if he or she knows of any groups. They might be able to connect you to organisations in your area.
This no-cost app for your mobile device offers helpful resources for those living with sickle cell disease. With the SCD Companion, you can:
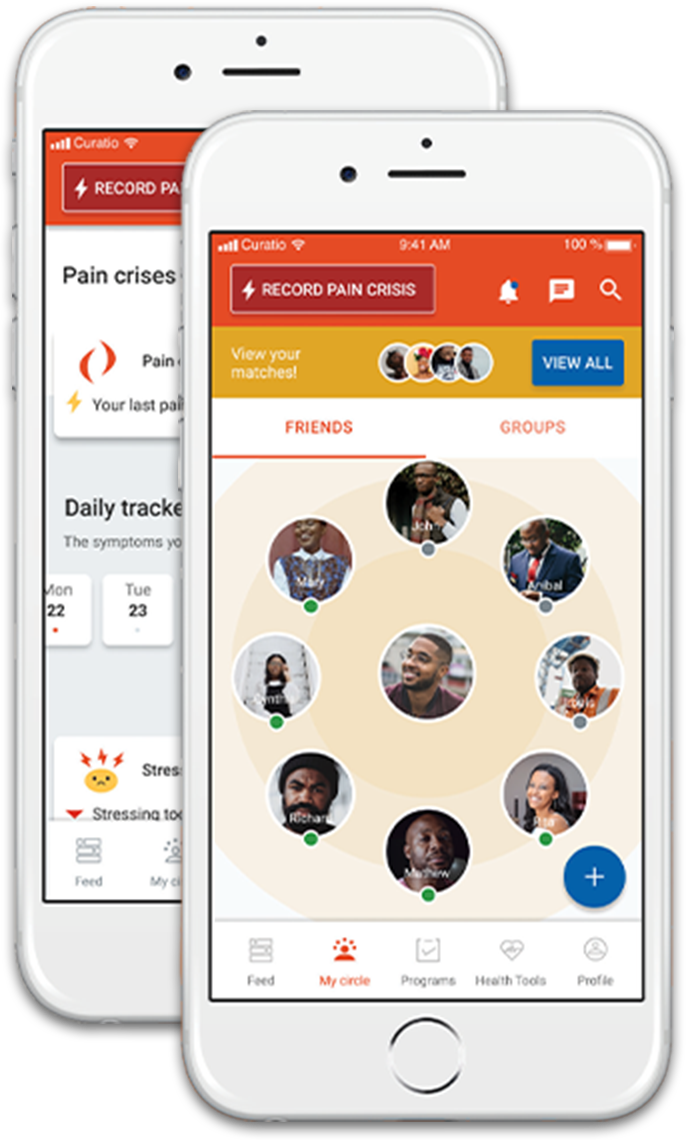
This app is sponsored by Novartis and was created by Curatio.